‘Atypical’ Meningioma
Welcome to Dr Khurana’s Atypical Meningioma page.
Images shown here are with the permission of Dr Khurana’s patients, for educational purposes.
For a YouTube video of meningioma surgery by Dr Khurana, CLICK HERE
Click image for larger view
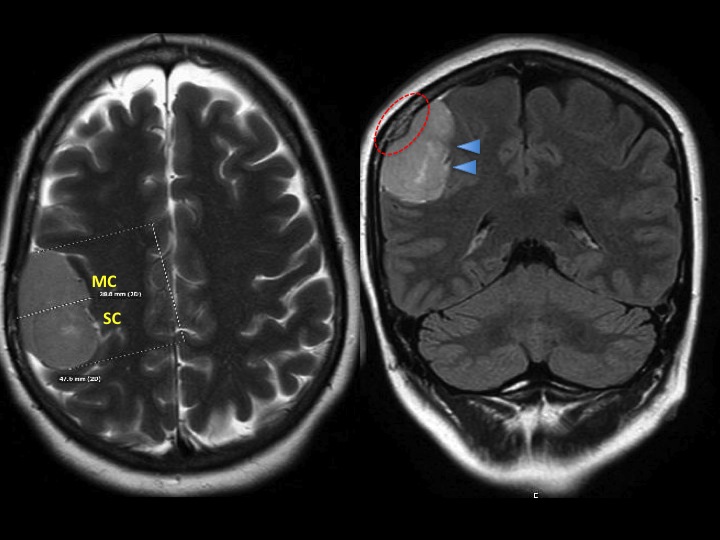
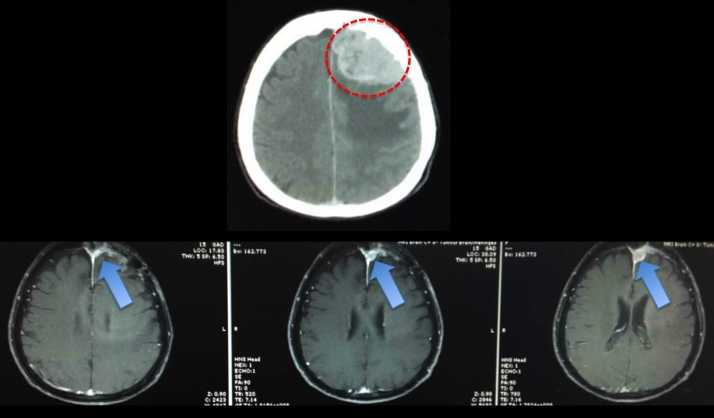
A meningioma growing and gradually displacing the right side of the brain over its “high-price real estate” (eloquent) primary motor cortex (MC) and sensory cortex (SC) regions is shown in the above MRI images. In the above right panel, the red dashed-circle shows a distinct area of reactive bone change in the skull overlying the meningioma (see image of skull, below). The blue arrow heads in the above right panel point to some regions of the brain that are compressed prior to any possible invasion by the mass. In such instances (large mass, ready accessibility, brain compression and possible early invasion), surgery should be favoured over radiation as the first-line treatment.
The right side image of a meningioma was found (following surgery and analysis of the pathology samples) to be “atypical” (W.H.O. Grade 2 – see pathology images and cellular features, below). An “atypical meningioma” has a higher tendency to grow faster, to recur following surgery, and to possibly adhere to and then invade surrounding tissues including brain, blood vessels and bone. Its complete microsurgical removal, along with any attached dura and abnormal overlying skull bone, is therefore important (see images, below).
There is some association between atypical meningiomas and chromosome 22 genetic abnormalities (e.g., monosomy 22 / loss of heterzygosity). Such abnormalities have also been noted in radiation-induced meningiomas and in Neurofibromatosis Type 2 (NF2) patients’ meningiomas.
This chromosome appears to contain a number of genes that may be involved in the origin of this particular tumour although it should be noted that most meningiomas diagnosed population-wide are “typical”, and “sporadic” (i.e., non-hereditary) in their cellular type and origin.
- Image 2
- Image 3
Click images for larger view
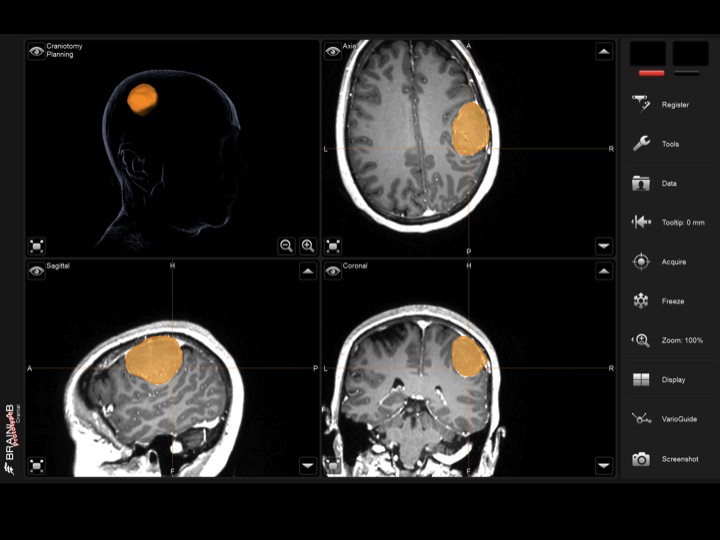
In the operating room, the 3-D colour volume rendering shown (image 2) was made via the Brainlab Curve neuronavigation ‘GPS-like’ system (image 3) that allows precise location and creation of the minimum craniotomy (surgical bone opening) required to remove the mass, while allowing tracking of surgical instruments whenever needed.
Microsurgical techniques are required for the complete and safe removal of tumours such as this, where there happens to be close adherence to and early invasion of the “eloquent” brain tissue.
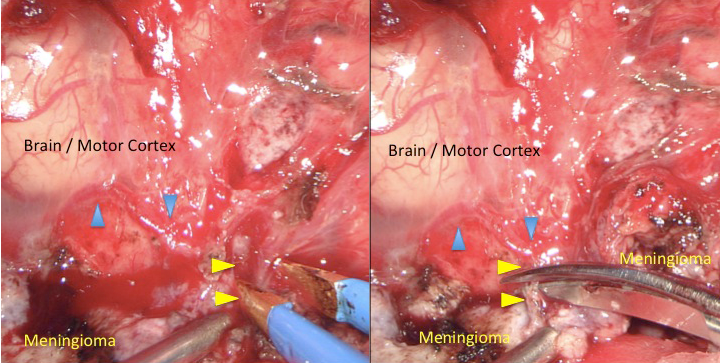
The intraoperative photographs shown to the right show how this particular meningioma’s tumour-vessels (yellow arrow heads) are sequentially surgically disconnected while the closely neighbouring and normal brain cortex vessels (blue arrow heads) are preserved.
These particular vessels are only 1 to 2 mm in diameter and the instruments above are “micro” tipped.
Click image for larger view
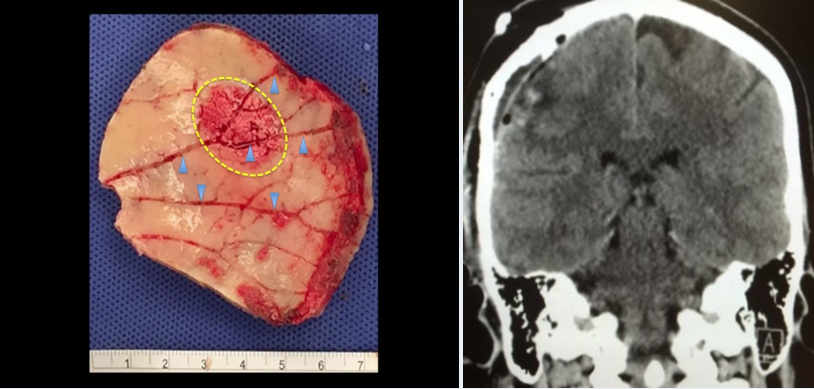
The left panel shows the effect this particular meningioma was having on the overlying skull bone, with thickening (hyperostosis) and hyperaemia (engorged vessels / dilated vascular channels; blue arrow heads), and a region of early bone invasion (yellow dashed-oval region).
The original bone flap shown on the left was replaced in the patient at the end of surgery, but the abnormal regions were first drilled away. The tumour was completely and uneventfully removed with the post operative contrast CT scan taken at 48 hours following surgery shown in the right panel.
Note the thin skull bone following drilling of its inner table.
Click image for larger view
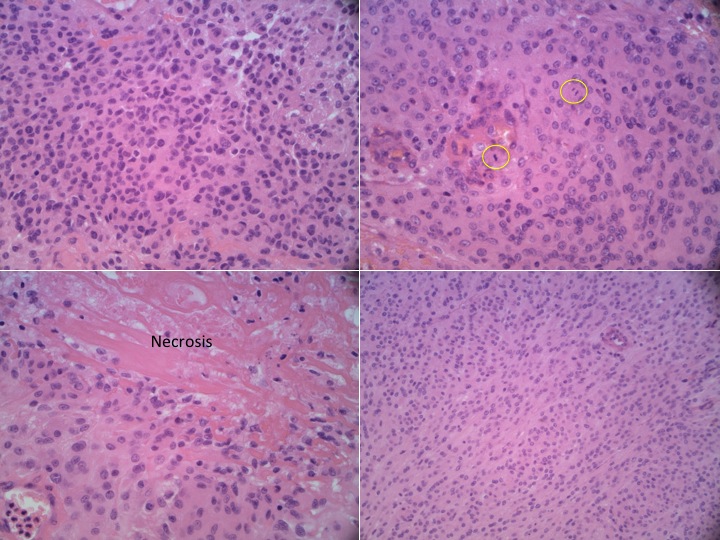
Pathology specimens from this particular meningioma revelaed “atypical” (W.H.O. Grade 2) features: hypercellularity (top left), mitoses (top right, in circles; areas of increased cellular division); necrosis (bottom left); and sheet-like low-cytoarchitectural regions (bottom right).
Despite the macroscopically complete “Simpson Grade 1” resection carried out here, the patient will be undergoing periodic radiological surveillance for any recurrence, which can happen more frequently with atypical meningiomas.
Repeat surgery and stereotactic radiosurgery can be appropriately reserved for recurrence should that ever arise.
Click image for larger view
The left collage show the sequential recurrence of an atypical meningioma over a period of less than 2 years following surgery.
In this situation, repeat open surgery followed by stereotactic radiation is an appropriate option.
Click image for larger view